|
|
|
This online tutorial series "Quality Improvement: Tool Time" reinforces practical
application of tools and competencies acquired during the live activity. Each Tool
is a combination of faculty commentary on essentials in clinical practice, links
to relevant scientific publications, and a printable handout that will serve as
a reminder. Please select the topic:
- Ensuring Quality of Care
- Optimizing Vancomycin for MRSA Infections
- Selecting Appropriate Therapy for ESBL- and KPC-Producers
- Dosing Strategies for MDR P. aeruginosa/A. baumannii Infections
- Adjusting Antimicrobial Regimens for Efficacy and Safety
|
|
Optimizing Vancomycin for MRSA Infections
|
MRSA's Changing Epidemiology
The spread of MRSA has reached epidemic proportions in US hospitals. Approximately 60%
of S. aureus isolates from hospitalized patients are methicillin-resistant. MRSA has
also spread into the community and is now a major cause of community-acquired skin infections.
|
|
Impact of Increasing MRSA
Prevalence
|

|
Dr. Conan MacDougall discusses
vancomycin MIC creep
|
|
|
Increasing prevalence of MRSA has resulted in a
significant rise in the use of vancomycin. From
2002 to 2006, a 43% increase in vancomycin use
has been estimated in 22 US institutions.
[1]
A potential consequence of increased vancomycin
use is a trend towards decreased MRSA susceptibility
to vancomycin, or “MIC creep”.
Though there is conflicting evidence for “MIC
creep”, it is widely acknowledged that vancomycin
effectiveness is reduced when the MRSA MIC
is 2 μg/mL or higher. This makes it critical to
- optimally use vancomycin to maximize
its effectiveness and safety
- recognize when an alternative agent is
needed
|
|
|
|
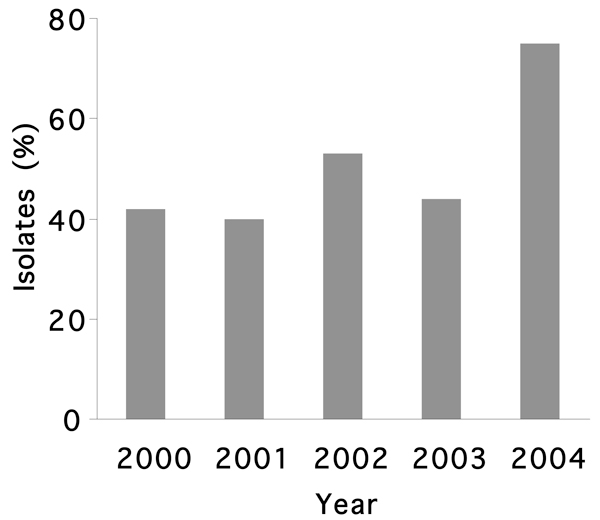
MRSA isolates (%) with MIC=1 μg/mL
[2]
|
|
Optimal Use of Vancomycin: IDSA, SIDP, and ASHP 2009 Guidelines
[3]
|
If MIC≤1 μg/mL, vancomycin is the preferred agent
|
Target AUC/MIC
|
400
|
Loading dose
|
25–30 mg/kg
|
Trough serum vancomycin concentrations
|
Obtained just before 4th dose
- >10 μg/mL for all patients
- 15–20 μg/mL for serious infections or if MIC=1 μg/mL
|
Dosage
|
15–20 mg/kg q8–12h for most patients with normal renal function if MIC≤1 μg/mL
|
|
If MIC>1 μg/mL, use alternative agent
|
|
Vancomycin at Higher Doses: A Threat to Patient Safety?
For serious infections or if MIC=1 μg/mL, the guidelines recommend trough serum vancomycin
concentrations above 15 μg/mL. However, this may come at the cost of increased toxicity. A
study by Hermsen and colleagues showed that patients with higher trough serum vancomycin
concentrations (>15 μg/mL) were 3-fold more likely to experience
nephrotoxicity (31% vs. 10% respectively; P=.04).
[4]
Though confounding factors may have
impacted this study with severely ill patients, clinical pharmacists should be aware of
the potential for nephrotoxicity when maintaining higher trough serum vancomycin
concentrations in their patients.
|
|
References
- Pakyz AL, MacDougall C, Oinonen M, Polk RE. Trends in antibacterial use in US academic
health centers: 2002 to 2006. Arch Intern Med. 2008;168:2254-2260.
Click here for complete article
- Wang G, Hindler JF, Ward KW, Bruckner DA. Increased vancomycin MICs for Staphylococcus
aureus clinical isolates from a university hospital during a 5-year
period. J Clin Microbiol.. 2006;44:3883-3886.
Click here for complete article
- Rybak M, Lomaestro B, Rotschafer JC, et al. Therapeutic monitoring of vancomycin in adult
patients: A consensus review of the American Society of Health-System Pharmacists, the Infectious
Diseases Society of America, and the Society of Infectious Diseases
Pharmacists. Am J Health-Syst Pharm. 2009;66:82-98.
Click here for complete article
- Hermsen ED, Hanson M, Sankaranarayanan J, Stoner JA, Florescu MC, Rupp ME. Clinical
outcomes and nephrotoxicity associated with vancomycin trough concentrations during treatment
of deep-seated infections. Expert Opin Drug Saf. 2010;9:9-14.
|
|
Suggested Reading
Lodise TP, Graves J, Evans A, et al. Relationship between vancomycin MIC and failure among patients
with methicillin-resistant Staphylococcus aureus bacteremia treated with vancomycin. Antimicrob
Agents Chemother. 2008;52:3315-3320.
Click here for complete article
This retrospective cohort study included 92 patients with MRSA bloodstream infection treated with
vancomycin. Infections caused by isolates with high MICs (≥1.5 μg/mL) were associated with
poorer outcomes compared with infections caused by isolates with low MICs (<1.5 μg/mL).
Mermel LA, Allon M, Bouza E, et al. Clinical practice guidelines for the diagnosis and management
of intravascular catheter-related infection: 2009 update by the Infectious Diseases Society of
America. Clin Infect Dis. 2009;49:1-45.
Click here for complete article
These 2009 updated guidelines by the IDSA replace the previous 2001 guidelines. They offer
evidence-based recommendations for clinical questions related to the diagnosis and management
of catheter-related infections, including pathogen-specific management recommendations. For
MRSA infections, vancomycin remains the treatment of choice, though linezolid and daptomycin
can be considered as alternative agents.
Lodise TP, Patel N, Lomaestro BM, Rodvold KA, Drusano GL. Relationship between initial vancomycin
concentration-time profile and nephrotoxicity among hospitalized patients.
Clin Infect Dis. 2009;49:507-514.
This retrospective analysis was designed to determine the pharmacodynamic index that would best
describe the relationship between vancomycin exposure and onset of nephrotoxicity. A total of
166 hospitalized patients who were given vancomycin to treat a Gram-positive infection were
included. Analysis revealed that trough serum vancomycin concentration was the best indicator for
predicting nephrotoxicity.
|
|