|
Zero Tolerance for HAIs: Pharmacists Take the Next Step Towards Quality Improvement and Patient Safety
A Series of 10 Case Workshops with Antimicrobial Stewardship Meeting Simulation at 10 State SHP Annual Meetings
Healthcare Gap in HAI Management
HAIs impact 1.6 million people in US hospitals each year and are associated with high morbidity
and mortality (nearly 100,000 annual deaths), prolonged length of stay, and a
staggering $5.7 billion in healthcare costs. Despite mandatory HAI reporting along
with non-payment for hospital-acquired conditions, there is no specific guidance on
how hospitals can reduce the HAI rate.
Pharmacists' Role in HAI Management
Stewardship principles are critical for appropriate HAI management. There is an
increased importance of the interdisciplinary healthcare team—physicians and
pharmacists—caring for and managing patients with or at risk of HAIs.
Pharmacists are being asked to lead the HAI management efforts by partnering with
physicians and contributing to the decision-making process to ensure quality of care
and patient safety. In particular, pharmacists have to apply the antimicrobial
stewardship principles to optimize the use of available agents and maintain their
effectiveness for current and future infections.
Initiative Learning Objectives
Learning objectives of this Initiative are specifically defined to address pharmacists’ needs in HAI management:
- Describe the prevalence and impact of bacterial resistance in HAIs
- Evaluate antimicrobial dosing strategies that minimize resistance development and achieve optimal outcomes
- Recognize how health-system pharmacists can play an active role in quality improvement and patient safety
with respect to the management of patients with HAIs
|
Aim of the Initiative
To address process-related issues
in HAI management by
empowering health-system
pharmacists from 10 State SHPs
with practical knowledge to
successfully manage HAIs.
Read more about Practice Gap, Learning Objectives, Target Audience
|
Addressing the Healthcare Gap through Educational Intervention:
"Zero Tolerance" Initiative
The “Zero Tolerance” Initiative aimed to empower health-system pharmacists with practical
knowledge to successfully manage HAIs by addressing specific process-related issues in HAI
management.
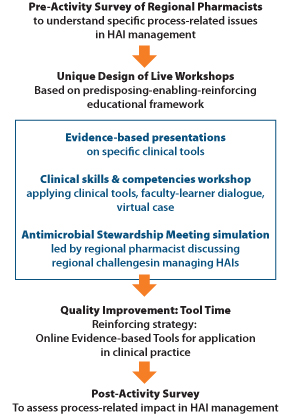
Indepth Pre-Activity Interview Survey of regional pharmacists along with expert consultation
resulted in design of the live program at 10 state SHP annual meetings. The Initiative
reached over 1500 healthcare professionals across the United States.
During the Live Workshop, evidence-based scientific presentations were followed by a case
workshop where faculty and learners partnered to address issues in managing HAIs. The case
workshop allowed formative assessment and presented opportunity to address learner knowledge
and competence gaps by putting scientific evidence in clinical perspective. Learner
experience was further enriched through ‘antimicrobial stewardship meeting’ simulation.
The simulation provided a real-world preview of barriers healthcare professionals face
while implementing stewardship practices and policies.
See Post-Meeting Reports
Formative assessment during the live workshops and summative assessment of evaluations
were used to design the reinforcing strategy Quality Improvement: Tool Time. This online
tutorial series reinforced practical application of tools and competencies acquired
during the live activity. Each Tool was a combination of faculty commentary on essentials
in clinical practice and links to relevant scientific publications.
See Tools
This was followed by a detailed Post-Activity Survey to assess specific process-related
changes adopted by healthcare professionals.
|
Faculty feedback
"provides participants with an opportunity to witness how complicated back-room
discussions can help pave the way to implementing important stewardship policies
at institutions."
"a unique approach . . . helps participants understand both the formal and
informal process of implementing new policies at hospitals."
Participant feedback
"This approach is extremely valuable to my practice and increased
learning potential and retention."
|
Assessment of the Impact of the Educational Intervention
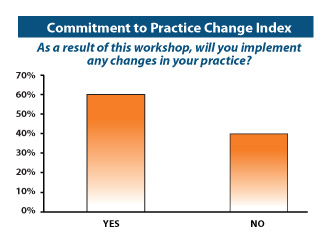
Commitment to Practice Change Index
Learners were asked if they intended to incorporate any tools suggested in this
initiative in their practice. About 60% of the learners committed to making practice-based
changes and specified changes they would incorporate in 3 months, 6 months, and 12 months.
|
|
Did Commitment Translate into Specific Practice Changes?
Learners committed to making practice changes, incorporated specific changes based on
direction provided during the Live Workshop and through Quality Improvement: Tool
Time. Majority of the respondents emphasized an improvement in their interprofessional
communication as a result of this Initiative. Other major areas on improvement were
antimicrobial selection and dose adjustment based on patient factors.
Insight Into Institutional Processes Related to HAI Management and Barriers
Institutions are moving in the right direction in optimal HAI management as evidenced
by increased emphasis on antimicrobial stewardship efforts at majority of institutions.
However, barriers to optimal HAI management continue to exist. Fortunately, the nature
of these barriers as documented in this Initiative is such that they can be addressed
by targeted educational interventions.
|